- /
Editors note: This article was originally published in 2019 and has been updated in October 2020 with more relevant and accurate information.
Constantly emphasised, health workers understand and know the importance of hand hygiene in their profession. However, hospital acquired infections (HAIs) are still occurring. The link between not washing hands and hospital-acquired infections (HAIs) has been known for more than 150 years.
Sadly, hand washing compliance rates are nowhere near that general awareness benchmark.
Australian hospitals report an average of 180,000 HAIs yearly, leading to 1 in 10 hospital admissions being affected each year. This translates into 2 million additional hospital days, primarily caused by HAIs.
The implications? It’s not only extended hospital stays. A need for additional treatment and diagnostics arises – thus increasing costs. But it gets worse. HAIs have terrible health implications for patients and hospital staff.
This is mostly preventable. But you need good infection control procedures. And hand hygiene compliance strategies that are constantly monitored, improved and optimised.
The Australian National Safety and Quality Health Service Standards requires hospitals to review infection control measures periodically in order to minimise the risk of infections.
The costs are high and it’s in healthcare facilities’ best interest to put safety before everything else. Now, let’s take a closer look at the costs of hand washing non-compliance in hospitals as well as some potential remedies for it.
What Percentage of Healthcare Workers Do Not Wash Their Hands Before Examining Patients in Australia?
Frontline workers are well-aware hand hygiene is compulsory in a hospital setting. But how many of them actually comply?
Statistics warn us that only 67% of Australian medical staff wash their hands before making physical contact with a patient. The numbers decrease further after contact with a patient’s surroundings.
Hand Hygiene Australia (HHA) is the national program that measures compliance in hospitals in Australia. Its 2020 report shows hand washing performance results of 1052 organisations.
Below is the general HHA compliance overview for the first quarter of 2020.
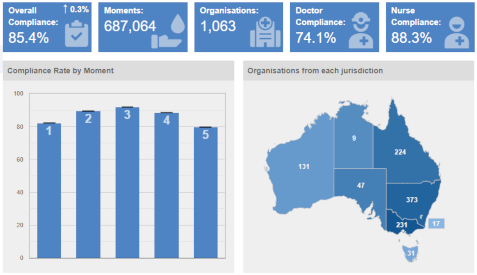
Image from Hand Hygiene Australia
The University of NSW study reveals such results may not be reliable due to the Hawthorne’s effect. A phenomenon marking the change in behavioural patterns when people are aware they are being observed.
Audits may prove satisfactory, but the results seem to dwindle after an audit cycle is completed. The study reports hand hygiene compliance rates plummeted from 94% to 30% once human auditors weren’t present anymore.
What Are The Costs of not Complying to Hand Washing in Australian Hospitals?
Not complying with the professional hand washing standard comes at a price. Hospitals should seriously consider the scope of negative outcomes associated with HAIs in their clinical practice.
So what are the actual costs?
Costs to the Australian Economy
Health costs are becoming a huge drain on the Australian economy. This is mainly associated with issues caused by obesity and mental health problems that have recently been on the rise. This has increased Australian health expenditures’ to up to $40 billion quarterly.
To narrow it down, estimated costs of surgical site infections can reach up to $268 million per year. While the total annual health care costs of bloodstream infections can rise as high as $686 million yearly.
Risks to Hospital Patients’ Health
HAIs are equally found in complex and urgent care centres as they are in day treatment centres and acute-care hospitals. Germs are transferred by medical professionals from one patient to another, mainly through their hands.
So, patients should be protected during the course of receiving their hospital treatment. And different management approaches should be tested to break the chain of contamination.
The most common HAIs are the following:
- Urinary tract infections (UTIs)
- Surgical site infections
- Bloodstream infections
- Gastrointestinal infections
- Meningitis
- Pneumonia
- Staphylococcus aureus bacteraemia
HAIs are the number one cause of the most common hospital complications. What unsettles the healthcare community is that a growing number of these infections are caused by multidrug-resistant organisms (MDROs).
But how do you deal with the rise of HAIs each year and an increase of MDROs? Nothing beats the continual investment in infection prevention and control which includes:
- Barrier precautions
- Screening of high-risk patients
- An effective hand hygiene promotion program
- High hospital hygiene standards
- Surveillance and reporting

Image from www.cdc.gov
Risks to Healthcare Workers’ Health
It’s critical medical staff are educated about the risks of acquiring HAIs. This is especially important for emergency care and intensive care unit workers. Medical staff should be aware they’re exposed to risks of acquiring infections such as Hepatitis C (HCV) or Human Immunodeficiency Virus (HIV) while performing their medical duties.
Medical staff should be educated about the transmission pathways of the various HAIs. Possible transmission methods include:
- Blood and body fluids that linger on equipment and can be absorbed by skin or mucosa
- Lung penetration of HAIs through the air
- Close contact with the patient
- Inhaling infected droplets
- Needlestick injuries
Therefore, good hand washing compliance plays a major role not only in terms of patient safety, but also in terms of medical staff safety. It also creates a safer workplace for your healthcare staff. Other standard precautions against transmission of HAIs include wearing:
- Gloves
- Protective mask
- Protective eyewear

Image from www.cdc.gov
Million Dollar Damages to a Hospital Budget
It remains difficult to figure out a single act of hygiene negligence and prove the hospital’s responsibility. Therefore, there’s a certain amount of complacency within hospital organisations.
However hospitals are still legally liable for protecting patients against life-threatening infections, with audits being more strict than ever. While, if the breach is successfully proven, medical negligence compensations can go through the roof.
Medical practice has seen cases settling with damages worth millions of dollars. And the lawsuits are on the rise. Below are a few examples of where hospitals were faced with a lawsuit due to hygiene negligence.
Example 1:
A 2015 case of a tuberculosis outbreak in Ontario, Canada where 400 patients were affected and was resolved in a generous settlement. The hospital paid out $1.7 million in compensation.
Example 2:
A hospital in Missouri, USA was penalised for an IV transmitted infection to a 69-year-old patient after suffering a heart attack. The hospital was obliged to pay $2.58 million worth of damages.
What Causes Hand Hygiene Non-Compliance in Hospitals?
With all this information available, why is there still a lack of adherence to hand washing compliance?
Understanding non-compliance with hand hygiene practices helps you fine-tune your improvement strategies. Now, below are some of the most common reasons healthcare professionals list for not adhering to good hand washing practices.
- They forgot or got distracted
- Empty soap dispensers at the sink and no hand rub available at the point of patient care
- Frequent need to enter or exit the room when sharing equipment or discharging and admitting patients
- Skin irritations due to the frequent use of hand washing products
- A misconception that wearing gloves implies there’s no need for hand washing
- A belief that the hospital protocol requires excessive hand cleaning
What Are Some of the Remedies for Hand Hygiene Non-Compliance in Australian Hospitals?
When you consider the costs, investing in hand hygiene compliance strategies seems perfectly worthwhile. But how do you devise a functional hand hygiene program? Especially when you’ve been cornered and defeated by barriers you’ve been witnessing in your everyday practice.
Every hospital and health care practise has encountered this problem before, but there are some strategies that have proven to be effective.
Hand Hygiene Australia offers support, systems and education materials for implementation of the National Hand Hygiene Initiative. The initiative is based on the WHO ‘My 5 Moments for Hand Hygiene’ which has been proven to help reduce the numbers of HAIs in hospitals.
The program suggests a multimodal system of hygiene management to be implemented across the organisation structure.
The strategies, which has been tried and tested in various demographics in the world, can be implemented in the following ways:
- Create an organisation-wide hand hygiene safety culture. Include all levels of your organisation structure, from individual healthcare workers to senior hospital managers.
- Invest in infrastructure that makes hand washing easy and convenient. Make hand washing facilities such as soap dispensers and alcohol-based hand rubs accessible in patient care areas.
- Promote hand washing compliance by including visual reminders such as hand washing posters.
- Educate and train your staff often.
- Keep track of your staff’s hand hygiene practices in order to identify areas of improvement. Then offer active performance feedback, strengthen leadership and reward positive behaviours.
Rise to the Hand Hygiene Challenge
Now, we’ve looked at the costs, causes and possible remedies of hand washing non-adherence, you’re able to plan a better and more realistic hand washing compliance program.
The simple truth is you won’t be able to gain control over HAIs until you hit the nail on the head. And what’s worse than not having enough control over factors that can endanger human lives and put your hospital at risk?
Only continuous efforts can make the difference. And a little bit of help from the outside can make it much easier for you.
Fresh & Clean can help you streamline your hospital hygiene workload by outsourcing your hygiene services.
But it’s not only that we’ll step in and help you handle your washroom supplies. We’ve made sure to profile our company as a one-stop place for hygiene in healthcare.
With us, you’ll have extensive support establishment-wise. We can cover you with our diverse rental programs, bringing professional hospital workwear, WH&S compliant first aid kits and clinical disposal bins right at your door.
Contact Fresh & Clean now and we’ll tailor our services to your specific needs.
Disclaimer: The information presented is not legal advice, is not to be acted on as such, may not be current and is subject to change without notice.






